People living in shelters or on the street, especially those addicted to opioids, navigate a new set of risks and challenges
By Katie Prout
On March 16, Neli Vazquez Rowland, president and co-founder of the North Lawndale, Chicago homeless shelter A Safe Haven (ASH), was working to transform an unused office space on the shelter’s first floor into a quarantine room capable of housing up to a hundred homeless Chicagoans ill with COVID-19. When we met, she waved a gloved hand at me before we sat down on couches six feet apart. Vazquez Rowland pointed to desks that would disappear, cubicle dividers that would become walls for “semi-private little rooms.” She expected a delivery of one hundred beds later that afternoon.
“We’re preparing for a surge right now,” Vazquez Rowland said. This was on the cusp of COVID-19’s news trend. Illinois had just over a hundred confirmed cases, and Governor J.B. Pritzker had yet to issue a statewide shelter-in-place order. A handful of individuals in the shelter had tested positive for COVID-19 and were quarantined to their rooms. ASH staff brought them meals and regularly checked in to see what else they might need. But the shelter was preparing for things to get much worse, not least because the population it serves is also at an increased risk for health issues related to opioid use.
Chicago was already in a public health crisis before its first case of coronavirus was reported on January 24: in 2018 alone, 793 people in the city died from opioid overdose-related deaths. (For comparison, the whole of Los Angles County lost 497 people the same year.) Opioid use is of particular concern for those living on the street and in shelters, who often lack access to adequate medical care and drugs like Narcan (generically known as naloxone), which can help prevent overdose deaths. As with coronavirus deaths, the number of opioid-related casualties in Chicago is highest among older Black Americans, who accounted for 53.6 percent of reported deaths in 2018.
Recently, Chicago has made progress in decreasing the number of opioid-related deaths. The city saw a small but meaningful decline of 1.4 percent in 2018, thanks to an ambitious 2017 plan from the state to lower deaths statewide by thirty-three percent within three years; millions in funding; and the dedicated work of harm reduction organizations like the Chicago Recovery Alliance, The Night Ministry, medication-assisted treatment (MAT) clinic workers helping those who want to manage their dependency with medication, and countless others all over the city. But things are precarious.
Harm reduction workers I spoke with are concerned that Chicago might be on the verge of a spike in opioid dependency-related deaths. If folks who rely on prescribed medications like methadone or buprenorphine to treat their opioid dependency are unable to access those drugs—either because they’re sick with coronavirus, their regular clinic is closed due to coronavirus, or their clinic is out of medication (a slim but real possibility, as we’re still experiencing a national shortage of methadone), they might go through withdrawal, potentially landing in an overburdened hospital, where they’ll be in competition for beds and resources. Or they might go back to street drugs to avoid withdrawal, accompanied by the usual risks of drug use, including overdose, Hepatitis C, and HIV.
One of the people I talked to was Dr. Steven Aks, who specializes in toxicology and emergency medicine at the busiest ER in Illinois. John H Stroger, Jr. Hospital historically treats higher numbers of uninsured patients than many other area hospitals, and offers outpatient treatment for opioid dependency. The hospital partners with MAT programs throughout Cook County, and is often is the first step for many into the world of medical treatment for their dependency. Someone who comes to the ER after a nonfatal overdose, for example, might be prescribed suboxone and provided with a referral to a Cook County clinic for ongoing observation, counseling, and care.
MAT meds are strictly monitored, but restrictions on how patients can take them have loosened. Usually, while suboxone can be prescribed for most patients in doses that will last them several weeks, patients who take methadone must visit their MAT clinic daily and swallow their medication within the clinic itself. However, on March 16, the Substance Abuse and Mental Health Services Administration issued new guidelines that allow clinics to use their own discretion and allow patients deemed “stable” to take up to twenty-eight days of medication home with them; those who do not fit this category can take up to a fourteen-day supply home.
Dr. Aks praised Cook County MAT clinics for the work they have put into making sure their patients have their medications. He also described seeing a worrisome drop in ER attendance from regular patients with opioid dependencies, even accounting for the new prevalence of take-home meds. “There will be major fallout in the substance community” in the months to come, he said, even if the shape of that fallout (needle-sharing diseases, overdoses) is as-yet unclear. “The thing I fear the most—you just hope the mortality doesn’t rise.”
I volunteer at the Chicago Recovery Alliance (CRA), an organization comprised of people living with HIV and drug use, health care workers, educators, and people like me who believe in providing a wide array of free services to anyone who wants to reduce drug-related harm in their lives and in their communities. Or rather, I did volunteer, until the organization paused all its such efforts due to COVID-19. (CRA staff still provide daily access to clean needles, condoms, fentanyl tests, and more throughout the city: for more information, call (312)-953-3797.) I miss the community and the work, and wanted to know how coronavirus is affecting opioid-dependent people living in Chicago’s tent cities, in their own words—specifically, their ability to get MAT meds, or street drugs, if they still use. So, last month, I covered my mouth and nose, put on medical gloves, and biked around asking people in the following communities how they were doing, careful to stay more than six feet away (I had not—and still have not—exhibited any symptoms of COVID-19, but I took additional precautions, just in case).
One of the first places I visited was the Belmont camp, a grouping of about twelve tents located under the mammoth Kennedy Expressway and encircled by a metal fence. It’s one of several “tent cities” set up by people in the city who, for one reason or another, have no place else to sleep. A Latinx man with shoulder-length black hair and cautious eyes stepped away from a grill he was tending and introduced himself as Junior. Junior is in recovery and relies on methadone to stay healthy. His clinic, like many in the city, is now open only three days a week. Every other day, he goes to the clinic and is given enough methadone to last him forty-eight hours. “It’s better than going every day,” he said. I described my fear of overdose increases. “Yes!” he said. “It could happen. It’s very possible.” But he hadn’t seen anything like that yet.
Another Latinx man joined us. He was on his way to work; he wanted to talk, but didn’t want to use his name, so I’ll call him Victor. Victor doesn’t use opioids; he tried, he told me, but they never really took. “What do you need, from the city or the public, to make it through this okay?” I asked. “A shower would be awesome,” he said. Before the virus, Victor showered at a nearby Planet Fitness, where he has a membership. Now that the gym had closed, showers were much harder to come by. But “people have been very good to us,” he said. “Water’s always here, food.” He showed me hand sanitizer, a portapotty, and two sinks that arrived from the city within the last three weeks. The portapotty is regularly cleaned by the city, he said, and the water in the sink is regularly restocked.
Victor needed to head to work, so he called over Willy, a funny, chatty man in his thirties wearing a ballcap and sweats, who introduced himself in a Chicago accent that I thought had vanished from the city. We talked for the next half-hour. Like Junior, Willy was now able to take his methadone home, though his clinic was still open every day, in case of emergencies. “I’ve heard people getting as much as eleven or twelve days, like twelve take-home bottles” of methadone, he said. That would be enough to help some stay home for twelve days before they’d need to return. “So far this weekend, they gave us two.”
“Us” is Willy and his dad, Enrique, an older man with whom Willy shares a fourteen-by-fourteen foot tent lined with shiny material he said came “from the airport.” Enrique is not a native English speaker, so he and his son go together to the methadone clinic on Elston and Fullerton Avenue, where Willy translates as needed. Willy has been a patient there for two years. Until take-home medication became available, he woke up at 5 a.m. most mornings, arriving at the clinic at 5:30 a.m., swallowing his medication in front of a clinic worker, then hustling to make it to his job at a car wash by 7 a.m. He works twelve-hour shifts. The move to take-home methadone helps him. “This way I’m able to get it, stay at home, sleep in a little bit later, you know, not be as tired from my shifts.”
The new take-home process is not without confusion. Clinics require people to bring back empty methadone bottles to access the next batch. The other day, according to Willy, Enrique forgot to bring his empty bottle with him, and the clinic worker he spoke with told him she couldn’t give him the next round. Enrique and Willy’s time-sensitive ride was waiting in the parking lot. Faced with the unpleasant possibility of withdrawal, and struggling to communicate with the worker, who didn’t speak Spanish, Enrique said, in English, “This is bullshit,” and walked out of the office. Willy, sitting in the waiting room, stopped him. With Willy’s facilitation, and with the help of a second clinic worker, both Enrique and his son walked away with the medication they needed.
Access to clean drug supplies, Willy told me, is the biggest challenge opioid users have due to coronavirus. A few days earlier, he and a few others from the camp had tried to exchange used needles for clean ones at a needle exchange two miles south, only to find the exchange closed, with no sign posted as to when it would reopen. William said that both the CRA and The Night Ministry have been sources of help, dropping off clean syringes and naloxone for the anyone at the camp who needs them, but the needles still pile up. Without more clean needles, William worried that hepatitis, already prevalent among current or former drug users in the city, will spread. “When you got like a thousand syringes in the tent from people who’ve come and used, you know, it’s like, what are you gonna do, you know? Then you’ve got like, twenty of us here with a bagful of ‘em, you know, and we can’t turn ‘em in.”
Worst-case scenario, Willy told me, if his MAT clinic were to suddenly close, “I would try to go to another clinic, see if I can transfer. Or, if worse came to worse, I would go to the hospital with one of my bottles, and I would show them the dose, and the day, and hopefully they’d be able to take care of me. And if worse came to worse around that, I know a couple of loopholes to get around medical procedures and all that. I’d go to a mental hospital, say I feel like hurting myself, they’re allowed to give you twenty [milligrams] of methadone like that,” he said. William trusts his clinic—it’s open nearly every day of the year, and if it does need to close, warnings are always posted two weeks in advance. But still, he said, he’s making plans—just in case.
The next camp I went by, on Chicago and Sacramento, is much smaller, much quieter, and much messier. At first, I wasn’t sure if it was still inhabited—Willy had told me that he heard this particular spot was recently disbanded by police. Seeing no one outside of the few tents there, I kept moving. (I only enter a camp if I’m invited, the same as with anybody’s home.) On the other side of the street, I met a white man in his fifties with a sunburn and unfocused blue eyes, carrying an empty bottle of Sprite. His name was Joe. Joe used suboxone, he told me, and was participating in newly-offered telehealth services, meeting with his prescriber over Periscope, Twitter’s live video-streaming app. Joe didn’t know what Periscope was, called it “a real pain in the neck,” but was glad to be able to bring his thirty-eight milligrams of suboxone home and take it in peace.
Joe lives in this camp, which has no portapotties, city-operated or otherwise. With the closure of all but essential businesses, he now has to walk a mile east to use the restroom of an open CVS. Joe said that, while outreach vans used to stop with clean supplies by two or three times a week, he hadn’t seen any in the last seven days. “You don’t happen to have fifty cents on ya, wouldya?” he asked me. I didn’t—I almost never carry any cash, but thanks to the CRA, I do always carry two kits of naloxone, the emergency opioid-overdose reversal medication that is administered via syringe or nasal spray. I offered him one. “Oh! I could use some,” he said. “I need it from time to time. Thanks.”
The last camp I biked to that day was mostly a series of open-air beds on Fullerton—in the beds, the still forms of individuals, blankets pulled over their heads. On the wall of the viaduct was a small, bright shrine to the Virgin. A lit Virgen de Guadalupe candle flicked below a poster of the same icon, doubled arms outstretched. To the right of the poster, in marker or paint, lines from the Hail Mary prayer were written:
Holy Mary
Pray for us sinners
Now and at the hour of our death
Amen
A few days later, Lloyd DeGrane, a photographer and harm reduction volunteer who has spent decades delivering clean supplies to people around the city, would tell me that the day I was visiting camps was within the same window of time when everyone he saw had, or was just recovering from, some type of dope sickness: “They’re in their tents, under their blankets, shitting and throwing up for a three- to five-day period,” he said. In the last month, people living in the camps lost their jobs, too, and there are no tourists on Michigan Avenue to ask for change. No money means no drugs, sending people throughout the city into the excruciating experience that is opioid withdrawal, DeGrane said. At first, the people he knows tried desperately to find drugs, to steal drugs, and/or to get into any MAT clinic that wasn’t already operating at full capacity. Those options quickly dissipated. “Now,” he said, “Their bodies and minds are telling them that this is the way it is.”
In March, Stephan Koruba, senior nurse practitioner at The Night Ministry (TNM), an organization that connects people experiencing homelessness and/or substance dependency to housing and healthcare (and can be reached at 773-256-7549), told me that the number of people he met with confirmed COVID-19 cases continued to be low, though within the two days prior to our conversation he had helped two young people with coronavirus symptoms get out of a congregate living situation and into stable—but isolated—housing. Koruba suggested that the stigma facing homeless people, especially if they use drugs, has, in this one instance, offered some protection. “People keep their distance from homeless people already,” he said. “They’re socially isolated—that’s the major problem we already face.”
When we next spoke, it was 8:15 p.m. on a Wednesday in May, and Koruba was driving into work. The situation has changed. It’s hard for people living in crowded shelters or encampments to socially distance, and, once the virus does reach members of the homeless community, it’s not easy to isolate them. The Chicago Reader reported that more than three hundred people at Chicago homeless shelters have tested positive for COVID-19. Julie Dworkin, policy director for Chicago Coalition for the Homeless, told the Reader that the precautions the city has put in place are “not adequate.” “There is not sufficient capacity right now to quickly address cases in shelters,” Dworkin said.
For the last five weeks, Koruba, two outreach workers, and another nurse practitioner have paired together for their one-night-a-week shifts—sometimes 11 p.m. to 2 a.m., sometimes 2:30 am until 5—manning a table set up by the Chicago Transit Authority (CTA) on the platform of either the southern terminus of the Red Line or the western terminus of the Blue. Wearing N-95 masks and gloves, each pair is able to provide a limited number of COVID-19 tests and a variety of harm reduction supplies. They also offer connections to a new telemedicine opioid-dependency treatment program, provided by Mile Square Health Centers, a program of the University of Illinois, for the people who’ve taken to sheltering each night on trains now almost entirely empty. According to Dr. Nicole Gastala, Director of Behavioral Health and Addiction at the Miles Square Health Centers, since the partnership with TNM began, sixteen people have started treatment with suboxone: of those sixteen, only two have stopped. “Which is really good!” she said, laughing. “Not just with this program; our whole no-show rate has gone down significantly, because [with the advent of telemedicine] we’ve taken away that transportation barrier.”
TNM is in cautious talks with the CTA to be allowed to provide nasal spray naloxone to anyone who asks for it from the platform table, and possibly even clean needle supplies. This type of city-supported opioid-dependency treatment and harm reduction action—meeting people where they’re at, not only metaphorically but literally, in public spaces—is unprecedented. “That’s why,” Koruba said, “even though we’re tired and everyone’s like, ‘you should take more time off’—and we should—we don’t wanna let these possibilities wither on the vine.” Continuing that metaphor, cross-partnerships allowing for wrap-around support are budding: Koruba assisted one COVID-positive person he met doing this work get housing at A Safe Haven, the shelter with the hundred covid-positive beds, to recuperate.
Two days after visiting the Belmont and Chicago camps, I borrowed my boyfriend’s car and drove south. There’s an encampment on Taylor and Kedzie, next to the CRA, where men in their sixties sit on a bench pulled from some long-gone minivan, playing music and cards and watching the street while Louise, an elderly, overweight Doberman mix who sleeps on a heated bed hooked up to a generator, sits at their feet and waits for pets. When I was volunteering at the CRA, I got in the habit of nodding hellos and goodbyes to these men, but we never exchanged more than a few words. Many of the people living in this encampment are Black, including Yolanda: a tiny woman with a lined, heart-shaped face, wearing a puffy coat. I’m five-four, but I could’ve looked down at the top of her head if we weren’t standing so far apart.
“I walked off my program ‘cause they’re not doing me right,” Yolanda told me. “They was too slow on giving me my medication. Like, I could never get over a forty [milligram dose]. And twenty and thirty is not doing nothing for me, ‘cause I’m feeling like I had using.” The methadone she received wasn’t enough, she said, to stave off dope sickness, and she was tired of asking for increases that still left her ill. She’s got naloxone from the CRA, but doesn’t have clean straws for snorting even though I know we have them. “So that can be in your story, too. How come every time we keep going to these places, we come back out and start using? What is this shit doing for us? That’s a story, too, right there.”
A woman with sunglasses, whom I’ll call Mary, leaned in when I asked what would help Yolanda survive. “What are those, the ones I call the strips?” she asked Yolanda. “Suboxone,” Yolanda said—then, to me, “She’s trying to get on some help.” Mary turned to me. “I work,” she said, “so I get the strip and do it myself. I know how.” She buys suboxone off the street. “Yep yep yep yep yep,” Yolanda said. “People selling to help each other, to make extra money.”
“Is it helping you?” I asked Mary. She nodded. One of the reasons federal guidelines have forbidden the use of take-home methadone or suboxone in the past is because of a fear people wouldn’t take their medication, and would instead sell it to others. To Yolanda and Mary, however, these sales are lifesavers. “Some don’t take it, and they know what they doing when they sell they shit,” Yolanda told me. “They don’t sell they shit if they need it real bad. They know other accesses, okay?”
When I ask how the coronavirus is impacting her, Yolanda showed me her small hands. “You see how clean my nails are? I wash these motherfuckers. I scrub ‘em.” She reached into her pocket and pulled out the mask she’s been wearing and re-wearing ever since she got it from a nearby hospital, during a stay earlier in the year, when she had pneumonia. She stands six feet away from people as much as she can. She gets clean straws for snorting from the nearest Dunkin’ Donuts, using her elbows to open the shop’s doors and washing her hands before and after she picks up the straws. The city had been by the camp, she told me, with food and water, but she didn’t take it. “There are people that really need it,” she said. “I do too, but I have access to money sometimes to go buy these things, know what I’m saying? I don’t take away from somebody that really, really needs it. I leave it be.”
At the end of our conversation, I asked her again what name she wanted me to use for attribution. Her face was set, serious. “Yolanda,” she said, and spelled it. She spelled her last name, too. “This is my real name. Put me out there.” I told her I would. But later, I chose to not include her last name, because I described her using drugs and I want to keep her safe—or at least not put her in harm. If I see her again, I’ll tell her that: even though I went against her instructions, I hope I did the right thing.
She’s got clout, Yolanda told me. Drop her name, and whatever camp I go to around here, I’ll be okay. With my white skin and my microphone, she said, I stood out. But mention her, and people would be open to talk to me. Mid-advice, she asked if I had a car I could use to get around to different sites. I told her I did, thanked her, and began to turn away. As I reached to pause the recorder, she added: “Because I will walk with you. If you need.”
The way she said it—after all her laughing and swearing and asking of questions—sounded almost shy. “Thank you,” I said. “That’s really kind.” I told her I’d be okay and promised to stop by again soon to see how she was getting along. And then we said goodbye, and promised each other that we’d try to stay safe. ■
Katie Prout is a freelance writer in Chicago. Her work has appeared in Longreads, LitHub, and elsewhere.
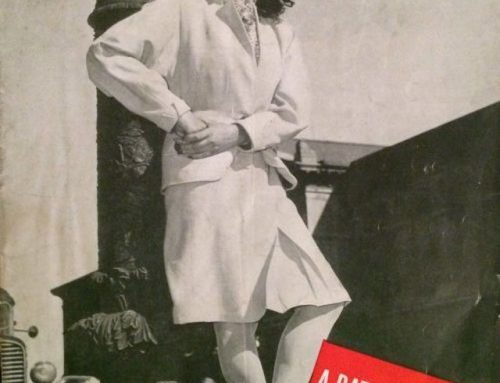
Cover image of Hope, who lives in Chicago and does not use opioids, by Lloyd DeGrane.
Belt Magazine is a 501(c)(3) nonprofit organization. To support more independent writing and journalism made by and for the Rust Belt and greater Midwest, make a donation to Belt Magazine, or become a member starting at just $5 a month.