Soon, nurses saw the gulf widen between their values and those of an increasingly commodified healthcare system.
By Eva Rosenfeld
“Why do nurses strike?”
A nurse and state union leader named Nadine Furlong delivered a speech with this title at a 1984 ethics conference sponsored by the University of Michigan. Furlong was exasperated with the question, or at least the underlying accusation, which seemed actually to be “Why do nurses strike when the right to strike conflicts with the duty to care?” Such an inquiry was laced with “erroneous assumptions,” she said. It assumed that the nurse has duties in the hospital that transcend the standard employee-employer relationship. It assumed that these “unsubstantiated duties” negated the basic societal right of employees to challenge chronically unsafe workplaces: in her view, the true source of harm to patients.
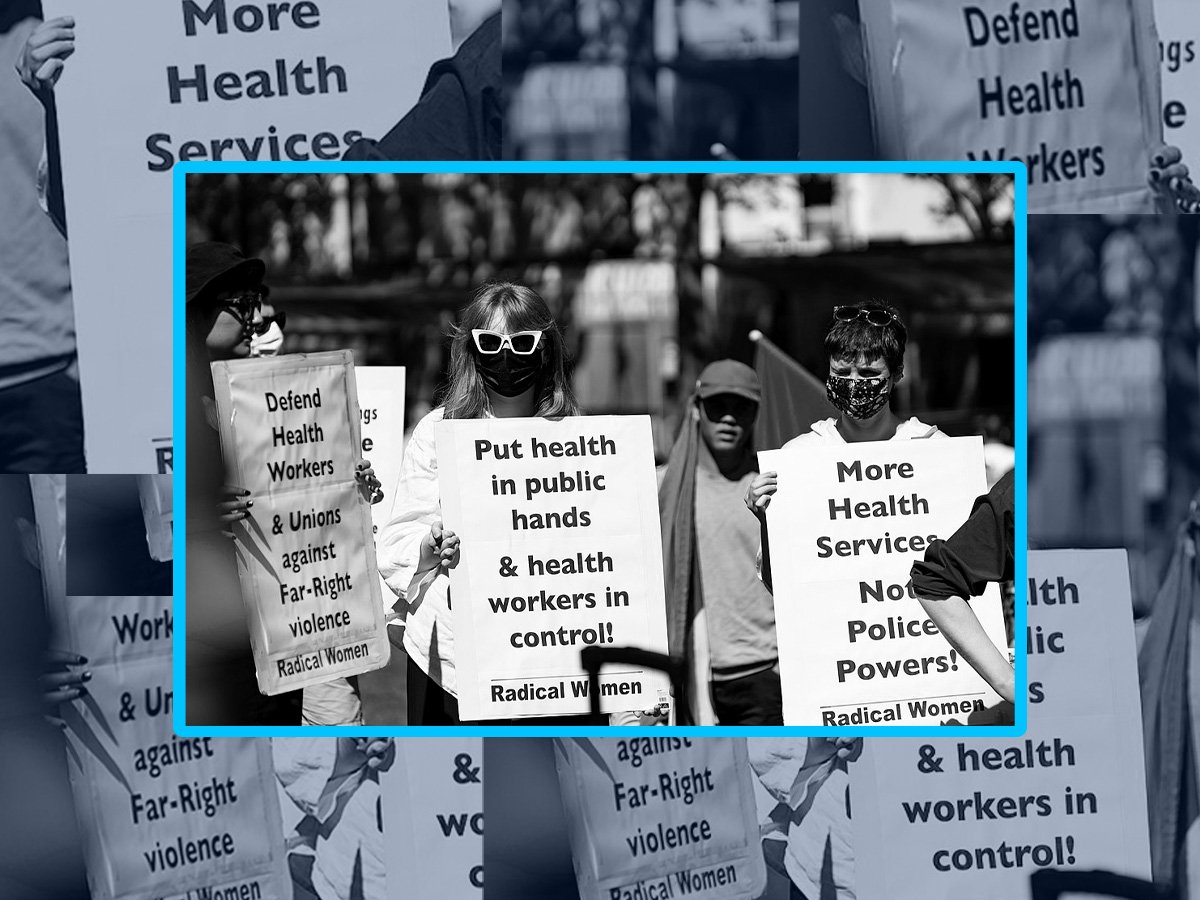
Asserting this right has been the basis of the nursing labor movement, which has grown in strength over the past two years. Nurses, mostly those in unions affiliated with the country’s largest nursing labor organization, National Nurses United, have organized strikes and labor actions across the country in response to ever more debilitating work conditions amidst the pandemic. Healthcare workers made up almost half of striking workers last year, mainly nurses and lower-paid support staff. They emphasized demands for “safe staffing” and protested “chronically understaffed” workplaces, where caregivers continually find themselves torn between patients, forced by time constraints to deliver compromised care.
In summer of 2022, nurses at the University of Michigan were particularly understaffed, stretched thinner because the hospital had laid off 738 support staff early in the pandemic to counter projected income loss. The hospital rebounded the next calendar year, profiting millions, but never rehired the workers. Short-staffed, managers enforced “mandatory overtime,” creating an uncompensated on-call system to fill gaps on the hospital floor.
It was the kind of desperate scenario that pushes nurses to the picket lines. The University of Michigan Professional Nurses Council (UMPNC), an affiliate of the Michigan Nurses Association at the state level and National Nurses United at the national level, authorized a “work stoppage”—it is illegal for public employees to formally strike in Michigan—and sued their employer. They ultimately won contract language that enforced nurse-to-patient ratios and ended mandatory overtime, clauses they hoped would return the burden of staffing the hospital to management. It was a solid victory on a set of issues that had plagued their workplace since at least the time Furlong took to the stage to correct the record on union nurses’ motives.
In fact, the problems University of Michigan picketed over in summer 2022 were remarkably similar to those they described in the 1980s. Responding to a 1981 survey over work conditions, nurses wrote:
“We’re chronically understaffed.”
“We have much mandatory overtime, and very sick patients. And NO extra staff to call upon in emergencies.”
“We are tremendously overworked to the danger point of unsafe patient care.”
“I hate to watch competent, highly skilled people leave out of sheer overwork and frustration; to save their very sanity.”
Any time a hospital lacks the capacity to care for all the patients who need treatment, newspapers tend to attribute the problem to a nationwide nursing shortage, as they did in the 1980s and again during the early days of the pandemic. Nurses’ unions today have been quick to counter that there is not a shortage of nurses, but rather of desirable workplaces. A March 2022 study from the American Nurses Foundation found that over half of U.S. nurses are considering leaving their jobs “due primarily to insufficient staffing, work negatively affecting health and well-being, and inability to deliver quality care,” while other studies have placed this figure as high as 90 percent. The labor supply in nursing varies dramatically across regions, and sometimes it can impact hospitals’ ability to hire, but understaffing persists in every kind of hospital, regardless of the labor market. Heidi Shierholz, president of the Economic Policy Institute, writes of a ubiquitous dynamic in which “Employers post their too-low wages, can’t find workers to fill jobs at that pay level, and claim they’re facing a labor shortage.”
Nurses share many complaints with workers in general, whose mass discontent has collectively sparked the “Great Resignation” and a spike in labor organizing. But unlike employees of most industries, who have organized around their own physical and economic precarity as they try to stay alive and afloat in the pandemic, nurses’ unions, with their clarion call for “safe staffing,” point to the precarity of their patients as evidence of a broken system.
Why do nurses strike? In Michigan, nurses’ unions formed in the shadow of auto unions, but faced a unique set of challenges as they defined their values and struggled for labor rights. Many of these obstacles were imposed by gendered stereotypes about nurses’ work; others stemmed from the emotional and moral issues endemic to caregiving. After all, a nurse fighting for a better workplace faces a different human equation than a trade worker. A nurses’ union represents its workers, too, but “we have that third person,” she says, “a third piece in our union that others don’t”—the patient. “And your decisions, how you can do the work that you are accountable in your profession to do, affects that person’s life, and their future.”
***
The discontented nurses of 1981 were a new kind of healthcare worker, armed with new labor rights and fresh insights from the feminist movement. They were also confronting a new kind of hospital. After the passage of Medicaid and Medicare in 1965, hospitals expanded across the country as insurance payments flowed into a healthcare system for which demand was steadily increasing. Healthcare consumption grew for many reasons, including an aging population. But in manufacturing hubs like Michigan or Pennsylvania, writes the labor historian Gabriel Winant, this growth was due in large part to the social dynamics of industrial decline.
As industrial labor won power in the mid-century, workers gained economic security, though much of their earnings came in the form of fringe benefits, like health insurance. As Winant explains in his book The Next Shift, which demonstrates how a contracting industrial economy gave way to a caregiving economy in the Rust Belt, these workers were able to take advantage of the healthcare system to meet basic social needs, like elder care and disability treatment. It was “a way of expanding the footprint of the welfare state without actually having to win any political victories,” Winant said in an interview.
Industries that depend on direct human service, like healthcare, childcare, and education, have certain fundamental properties, he explains. They are labor-intensive, they are in many ways more art than science, and, within them, there are hard, human limits to how much productivity can increase. And so, as healthcare services expanded from the late 1960s into the early 1980s, their growth was unavoidably labor-intensive. It was in hospitals’ interest to hire fast to meet demand. At the same time, they faced mounting external pressure from regulators to cut costs.
By the late 1970s, the federal government had begun to panic over the rising cost of healthcare, which bureaucrats blamed on the “overutilization” of care. The Carter administration deputized regional planning councils called Health Systems Agencies (HSAs) to reduce services. This convoluted regulatory regime was never terribly effective, not least because HSAs often had goals that contradicted their official mandate. Local officials serving on these councils, for instance, saw that hospitals were becoming crucial sites of employment and investment in deindustrializing areas that otherwise faced a sharp decline in economic activity. Healthcare costs have been viewed nationally as a fiscal problem, but health care inflation “represented, ironically, a political solution to the ravages of deindustrialization,” writes Winant.
By the mid-80s, cost-cutting would radically restructure the hospital environment. But even by the late 1970s, with austerity politics in the air, hospitals anxiously searched for savings in their growing wage bills. They lowered pay, but also assigned more patients to proportionately fewer workers, and redistributed technical tasks to lower-paid tiers of employees.
Nurses were an easy target. Until the mid-20th century, hospitals “were just not used to paying for nursing care,” says nursing historian Julie Fairman in an interview. Even after the days of religious nursing missions, hospitals depended largely on uncompensated nursing students in their training schools to make up their workforces. “Hospitals have always used nurses as ways to not just remain solvent, but to keep their economic overview as good as possible,” she says.
Most healthcare workers in the U.S. gained the right to collectively bargain in 1974, when an amendment to the National Labor Relations Act removed an exemption of the nonprofit healthcare industry from labor relations statutes. Yet in most states, including Michigan, nurses embraced this development slowly. In the 1980s, collective bargaining still remained “a subject of controversy” and “somewhat foreign to many nurses,” wrote Patricia Ibbotson, RN, in a 1981 issue of The Michigan Nurse, the publication of the Michigan Nurses Association. The profession was bogged down in its historical identity—what the American Nurses Association (ANA) then called the “you’ll get your reward in heaven” philosophy.
The 1974 amendments fueled fierce debates over the value of unionism. Across Michigan, nurses were torn between “the conflicting ideologies of a service-humanitarian orientation sometimes called ‘Nightingalism,’” after the famous nineteenth-century nurse, and “the desire to be assured economic security and recognition as a professional,” wrote one Detroit nurse, Phyllis Brenner, in 1983. What did it mean for a profession originating in religious volunteerism, long predicated on the uncompensated or undercompensated caring labor of women, to reverse course and make demands on their employers, even to strike?
Pro-labor attitudes spread as nurses took cues from the women’s movement to stand up for themselves in the workplace. Throughout the 1980s, columnists in the Michigan Nurse attempted to raise the consciousness of their colleagues. “Women, including nurses, have been told power isn’t ‘nice.’ This perception is inaccurate. Nurses are the key component in the healthcare delivery system in this country. They have the potential for great power,” wrote Ibbotson in 1981. “Collective bargaining is a useful adjunct in achieving a power base for nursing and a tool for professional growth.”
Dozens of other nurses penned similar appeals. Articles prepared nurses for grievance and arbitration processes, informed them of their rights under OSHA, and tried to rouse what was widely viewed as an apolitical group, describing tiers of participation from “apathetic” to “gladiator.” “Examine nursing curricula and note the lack of political content. However unintentional, conformity and docility have frequently been the affective student ideals fostered by faculty,” wrote two RNs in 1983, a time when 98 percent of nurses were women. But reconciling the identities of “caregiver” and “laborer” remained a difficult task, even for unabashedly pro-union nurses.
These issues came to a head in 1981, when the University of Michigan nurses held their first “work stoppage,” lasting 23 days. Just over half of the hospital RNs walked out. A report created after the strike by outside consultants, hired by hospital management to conduct a “healing project,” documents the reactions of nurses from both sides of the picket line. Nurses who worked through the strike accused strikers of perpetuating a “negative uncaring image.” Both sides called the others “traitors.”
They sparred with particular animation over the meaning of “professionalism,” a term that proved flexible enough to represent any view of collective bargaining; those who supported it and those who opposed it both claimed to be fighting for their professional values. Unionism was not exactly popular among nurses, and its critics tended to take the position that professionals didn’t join unions, that collective bargaining was a blue-collar tactic belonging to the trade unions, which, in Michigan, always meant auto workers.
Nadine Furlong, in her 1984 speech, represented the opposite view: “The argument to work it out ‘professionally’ flies in the face of fact,” she said. “Nurses have acted ‘professional’, been ‘dedicated’ and had a just cause, for 100 years. During this time they have remained economically exploited and professionally liable for unsafe nursing care of patients due to inadequate working conditions.”
Still, even striking nurses felt conflicted about their identities:
“We didn’t really act like labor—the strike was quiet and peaceful.”
“No matter how hard I try, I can’t feel like an auto worker or coal miner.”
***
“Professionalism” took on contradictory meanings because it is, in Winant’s terms, “a contradictory phenomenon”— a designation for workers who participate in “some of the functions of management,” or at least exert some control over who gets to enter their profession. The socialist writer Barbara Ehrenreich and journalist Dierdre English criticized the drive to professionalize nursing altogether. At best, they wrote, it failed to challenge the gendered hierarchy of medicine. “At worst, it is sexist itself, deepening the division among women health workers and bolstering a hierarchy controlled by men.”
Like their detractors, union nurses used the term “professionalism” to distinguish their work from a less credentialed tier—not industrial labor, but “feminine vocations” like unpaid caregiving, domestic work, and lower-paid healthcare work. They wanted to stop being treated like a catch-all profession, the unofficial mothers of the hospital, expected to pick up what was left on the floor. In 1981, the UMPNC won a “Professional Nursing” clause. It defined what university nurses’ duties included and, maybe more importantly, excluded. Even today Michigan nurses point to this contract language to decline when they are asked, for instance, to start taking out the trash.
Pro-union nurses wanted just as much as anti-union nurses to be seen as professionals, but they saw unionism as a path to professionalism, not its antithesis. Real professionalism, to them, meant autonomy in the daily operations of nursing. This included higher nurse-to-patient ratios, control over how the hospital floor was staffed, and flexibility to make clinical decisions without a doctor’s supervision. A good contract, they believed, was the only mechanism with any teeth to gain these things, plus better pay.
Still, these concerns, so closely tied to the act of caregiving, felt distant from the goals of classic trade unionism. Striking may have been necessary, but that did not make the decision to leave a patient at the bedside less fraught or painful. Many of those who walked out in 1981 echoed the feelings of one nurse, who reported, “I was so frightened by walking a picket line and yet I couldn’t seem to figure out any other way to get better working conditions. I just kept crying all night before it happened.” Margo Baron, who founded the UMPNC, was known to remark, “Nurses never go on strike for money.”
Within the nursing establishment, unions had an uneasy foothold. Both the MNA and its national counterpart, the American Nurses Association (ANA), were “professional organizations” whose leadership consisted mostly of nurse higher-ups—executives or educators who did not provide direct care. The difference between a professional organization and a union had always been murky, but depended mainly on the familiar distinctions of status and expertise. ANA had been officially sympathetic to collective bargaining since the 1940s but maintained a no-strike position until 1968. The MNA, meanwhile, had a small labor arm with limited representative power whose goals often clashed with those of managerial nurses at the helm.
As deindustrialization eroded the membership of Michigan auto unions, some tried to recruit health workers into their ranks. But many nurses felt that these invitations were themselves a threat to the ideal of “control over practice.” Joan Guy, an MNA executive, chided nurses who wanted to take advantage of the clout and resources of established unions. They were already struggling to overcome “the domination of nurses as women by medicine, health agency administrators, insurance leaders and legislators (mostly men),” she wrote. “Yet large numbers of nurses appear willing to transfer the determination of their employment and professional rights to still another type of male domination—the labor union. How ludicrous and self defeating! Do we really have to have ‘big daddy’ do it for us?”
Many union nurses felt more affection for their industrial counterparts but still strongly favored a discrete nurses’ union. There were, after all, life-or-death issues on the bargaining table. They needed representatives who understood the medical and interpersonal dimensions of the job. Diane Goddeerian often uses the figure of “seven minutes” to illustrate how long a caregiver might have to intervene after a traumatic event before a patient faces irreparable changes. Can you get to the bedside? Can you get a doctor? Can you get the ancillary staff and equipment necessary to intervene? Are you disoriented at the end of a mandated double shift? Someone’s life course is at stake, Goddeerian says, and “there’s no turning back if the seven minutes go by and you weren’t there to take care of them.”
***
Soon, nurses saw the gulf widen between their values and those of an increasingly commodified healthcare system. The Reagan administration spurned the era of regulatory cost-containment, instead imposing price mechanisms to allow market competition to structure the healthcare industry. This led to economic polarization in the healthcare industry, forcing many community hospitals to merge or shutter while prestigious hospitals continued to expand, and setting the stage for healthcare conglomerates to grow and consolidate. One of the most significant changes was the prospective payment system, a 1983 insurance reform that further incentivized hospitals to direct money towards high-intensity illness care and away from any sort of care that wasn’t illness-treatment—like the comprehensive care that nurses provided.
Even as hospitals needed nurses to achieve outcomes they could be reimbursed for, they increasingly viewed nurses as a cost, rather than a source of revenue. The structure of Medicare and Medicaid did little to contradict this view. MNA nurses complained in a 1984 statement that third party reimbursement policy hindered “the demonstration of the cost effectiveness of nurses in providing health care,” partly because its paper trails attributed outcomes of nursing care not to the nurse, but to the supervising physician. Hospitals have still collected little data, or don’t really want the data, about what revenue nurses generate, says historian Julie Fairman. Time and time again, this omission has justified minimizing costs in all aspects of nursing, from staffing levels to educational opportunities to wages.
The rallying cry for fair wages among nurses in the 1980s was the idea of “comparable worth”: that workers were undervalued in industries where traditional “women’s work” predominated. Today’s correlative, the “wage gap,” conjures images of managers covertly paying women less than men in the same roles. “Comparable worth” had a slightly different orientation, emphasizing how certain kinds of labor were treated or mistreated in the capitalist labor market. “The wage and salary concerns of all women are embodied in the wage and salary concerns of nurses,” wrote Furlong in 1984. “No other female occupation provides such a glaring example of the failure of market forces to determine appropriate wage rates.”
That hospitals continually wrote off nurses as a line cost, or even as part of “the room charge,” as one Michigan nurse put it, demonstrates the same effect: how labor deemed “women’s work”—whether or not performed by women—is systematically devalued because it is viewed, like housework, as the backdrop that sustains productive activities, and not a productive activity in and of itself.
Facing an increasingly medicalized healthcare landscape, the “professional” label took on a new weight. It seemed like a way to possibly, finally, define nurses’ labor—not only for the sake of recognition, but to make it visible on the hospital’s revenue statement.
“Nurses have had a hard time establishing their professional identity because medicine is based on outcomes, and it’s hard to quantify outcomes from nursing practice, although there are clearly outcomes from nursing practice,” says Anne Jackson, who started her nursing career at the university in the mid-‘80s. As an ambulatory care nurse, she explains, hospitals would like to quantify her by the number of phone calls she makes. But caring labor, no matter how expert, is existentially hard to define.
“Yes. You give the medicines. Yes. You take the vital signs. Yes. You monitor the patients,” says Jackson. But really, the nurse “is kind of like a MacGyver. Here is your patient with this problem. I’m not going to say what medicines they need. But they’ve got to figure out how to deal with this disease in their life. And it’s the nurse that helps them figure out how to do that. What is your socioeconomic status? What is your education status? What is your health literacy?”
Jackson recently asked a pediatric patient what she was doing in the hospital. The girl’s father was angry at the question, which was, in his view, needless. The doctor had already come in and diagnosed the problem.
“I knew why she was there,” says Jackson. “I wanted to know what she knew. And so I was just sort of using the Socratic method to figure out what she knew, how she understood, what information I still needed to give her, without being rude and just blabbing at her.”
In 2017, the “University of Michigan Health System” became “Michigan Medicine.” To Jackson and many other nurses, the name change signified the culmination of a long arc towards commodified medicine, “making us completely medicine-driven, as opposed to a much more collaborative institution,” she says. It felt like evidence that their contribution was no longer valued at the institutional level.
***
In 1989, Deborah Stoll, a young intensive care nurse, walked to the UMPNC offices in Ann Arbor, near the hospital. She wanted to talk to Margo Baron, the union’s chairperson. Stoll had struck in 1981, but had not known the ins and outs of bargaining. She was a young nurse, “showing up for work and having a good time and dating and putting money in my bank account.”
Baron was busy preparing for the UMPNC’s second work stoppage. The hospital was short-staffed and “stuffed to the gills,” one node in a nationwide nursing shortage. Stoll remembers receiving notes from admissions: “Fifty-some patients admitted today and we have four open beds. Have a good day!”
Managers used mandatory overtime to respond to the shortage, forcing nurses, many of whom were responsible for children at home, to stay on without warning. Shifts were rearranged at will, from night to day or day to night, so workers could not plan patient care in advance, and sometimes found themselves working back-to-back shifts of up to twelve hours each, too tired to think straight. “Most everybody learned not to answer their phone because that could be their nurse manager on the phone telling them they had to come in on their day off,” says Stoll. “Everybody bought answering machines.”
Nurses reported a cycle of exhaustion, stress, and unsafe care. “A lot of it was the same issues that we’re having now with short staffing,” says Jackson.
Stoll asked Baron if she could help with anything, and Baron had her call nearby hospitals to send nurses to work in the event of a strike. Stoll became wrapped up in the collective bargaining process. Her knowledge grew. Her attachment to Baron grew: “I think, somewhere in the back of her mind, she chose me as her predecessor without telling me that.”
This time, eighty percent of the university’s RNs walked out. They demanded that management end mandatory overtime and staff the hospital floor at levels appropriate for safe patient care. By striking explicitly over staffing, nurses had found a locus for their concerns as workers and caregivers. The demand for staffing ratios explicitly linked the interests of the worker to those of the “third person” in nursing labor negotiations—the patient.
Ultimately, the union won a large wage increase instead of improved staffing language. It was hard to say whether the money got to the heart of the matter; it temporarily raised staffing levels by attracting more nurses from around the region. Other hospitals across the state were forced to raise wages in response. The victory was meaningful, but ephemeral.
There was an agreement, for a few years, between employer and union, that two strikes in nine years had been too much, with no real victors. Together they tried something unusual in the field: they transitioned to “mutual gains,” a less confrontational, more consensus-based approach to bargaining. Stoll had become a spokesperson during the strike. “And then Margo appointed me to continue on with the bargaining team after fact-finding,” she says, “so I did that. And then she asked if I would run for chair, and I did that.”
She was grateful that the shift to mutual gains coincided with her tenure as chair. She felt she could not survive the head-butting of big, traditional labor negotiations. “Compromise was part of my career, part of my internal core,” she says. “But it is not easier, let me tell you. It is not easier at all. It’s very time consuming and very difficult.” For a few years, nurses and management collaborated to promote nursing autonomy and prevent the workload issues that had prompted the strike. But then, says Stoll, mutual gains “just became harder to do.”
***
By the 1990s, the nature of healthcare labor was transformed. Healthcare systems began warring with insurance companies over rates. Hospitals responded to the pressure by “restructuring”: a mass adoption of “lean models” of medicine and “just in time” policies, practices borrowed from industrial manufacturing to operate using the minimum amount of resources. Even wealthy university hospitals that had avoided the effects of a staffing crunch in the previous decade felt one now.
At the University of Michigan, as time dulled the acuteness of the strikes and administrators turned over, “it became harder to get the buy-in from management, who had things they wanted, and didn’t really care why we didn’t like them,” says Stoll. “They were sliding back into a more traditional bargaining process, and I think they’re firmly there right now.” Nurses lost interest, too. “Sometimes you just want to get mad and get even, and mutual bargaining doesn’t allow that.”
Over the next decade, the ANA also became less sympathetic to labor. Its nurse manager leaders disliked the strong influence of traditional unions and aligned its priorities increasingly with hospital administrations. By 2008, its leadership proposed a change in its bylaws which would effectively disenfranchise its labor arm, the United American Nurses (UAN). In the past, member organizations had paid their dues to the ANA, and a large portion went towards labor representation. Under the proposed bylaws, dues would remain the same, but would no longer fund bargaining. The state organizations faced a financial ultimatum to choose between the century-old institution and the now severed labor arm.
The vote over the new bylaws was to take place at the ANA’s annual meeting of state delegates in Washington D.C. in 2008. Michigan, one of the UAN’s most active constituencies, was at the center of debate about the bylaws. The MNA’s president, Cheryl Johnson, also headed the UAN. But the MNA’s influence and morale took a sharp hit when Johnson died abruptly in October 2007. Her death left Diane Goddeerian, then a nurse at Sparrow Hospital in Lansing, to steer the state union.
In the months leading up to the vote and throughout the conference, UAN’s core members tried to propose alternatives. They felt hospital systems would be more empowered to conquer a divided nurse workforce. But they felt the absence of Johnson’s knowledge and leadership. Another disadvantage was that executive nurses were overrepresented in these conversations; because the conference was expensive and meant taking several days off work, most staff nurses could not attend. The Michigan nurses decided in advance to withdraw from the ANA if the delegates voted for the split. When it happened, they walked out of the conference and into the unknown.
I asked Goddeerian if she was there that day. “Now you just sent chills down my spine,” she replied, “because yes. I had to get up to the microphone and announce that we were leaving. I remember one of the phrases in that speech was, ‘ANA is a house with many rooms. But you’ve made it clear there is no room for the nurses in the labor union.’ And we were done.”
The choice to leave was divisive among nurses in Michigan. Friendships suffered. “It was hard to be in the middle because there was no middle,” says Goddeerian. But a few other union states left the ANA soon after, and California and Massachusetts had both left a few years earlier, and they had survived. “You just had to say, for the greater good, for the nurse’s voice to be heard in the workplace, we have to do this,” Goddeerian says.
California nurses had also achieved something new: they had lobbied successfully for minimum staffing levels to be written into state law, like those that governed the airline industry. If staffing ratios were legislated, unions would not have to renegotiate them in contract after contract. The state unions that had left the ANA joined with California and Massachusetts to start a larger push in the political arena—“Something that nurses have never been very comfortable with,” notes Goddeerian—to promote staffing bills at the state and federal levels.
This alliance became National Nurses United (NNU), today the largest nurses’ union in the country with a membership of about 225,000. In its early days, NNU agreed to partner with the AFL-CIO, reflecting the new union’s desire to cultivate broad solidarity and a voice in the national labor movement. There was a logic to the affiliation, Goddeerian says. After all, almost everyone in the AFL would spend some time in a hospital, and when they did, they would want to be safely cared for. Having them understand “our issues, understand what staffing ratios mean, it’s very important,” she says. “They might not have paid attention to it, because they’re working on their issues. Well, then our issues become their issues, too.”
At a hearing in the Michigan legislature over staffing legislation, Goddeerian remembers a committee member asking a nurse manager, who was representing the American Hospital Association, “Are there any staffing levels in the bill that you could agree to?” She said no, expressing the most common criticism from opponents of mandatory ratios: that nurses should use their professional judgment in the moment to act in the best interest of the patient. The two went back and forth. The committee member asked if the nurse manager could agree to a ratio of one nurse to one patient in the operating room, typically considered a common sense standard. She evaded the question: “Well, I think at the time we would look at that.”
Goddeerian remembers thinking, “Can’t you just do the right thing and say, ‘Well, yes’? And it didn’t come out.”
***
To this day, no “safe staffing bill” has passed in Michigan. Nurse-to-patient ratio laws exist only in California and New York. In recent years, state affiliates of the contemporary ANA, now widely perceived as a managerial nurse organization, have joined with the American Hospital Association to campaign against versions of this bill.
In the pandemic, the consequences of short staffing became more dire as nurses reached new heights of stress, exhaustion, and “moral trauma” from tending to life-or-death situations under needless conditions of scarcity. The ANA’s position on staffing has nonetheless become more ambiguous: on its website, it promotes “mandated nurse to patient ratios or standards,” but it does not support an NNU-backed federal bill which would establish them. The NNU, meanwhile, has emerged as a giant in the labor landscape of the pandemic, bearing the torch of the staffing demands that first took shape in the 1980s.
Looking back at the past decade and a half from a historian’s view, Fairman has noticed what she calls a “sea change” in nursing labor movement’s rhetoric on staffing. It has grown less focused on caregiving and the need to be properly compensated for it. Instead, it tends to point to a large body of research, conducted since the 1990s, demonstrating the inverse relationship between staffing levels and patient mortality. Unions have drawn on this evidence to emphasize patient safety, the idea that “if you don’t give us better working conditions, our patients are going to suffer,” Fairman says.
It may be that partnering with other national unions has helped nurses strategically identify where their power lies, and thus, how to situate their demands. Emphasizing that “we care for you” has never served American nurses very well, Fairman says. “’Patient safety’ is a less gendered term and actually gets more public recognition.”
Nurses’ political messaging has required the same principle of self-sacrifice as their old professional mandate. “It had to be more about the patients than about the nurses themselves,” Fairman says.
The MNA’s wins have become more frequent and more substantial. Lately, it has had the most success unionizing nurses in the Upper Peninsula, where most of the hospitals are relatively small. It is becoming more and more difficult to organize large corporate hospitals with money to pour into union-busting efforts. The long shadow of the profit-driven consolidation of the ‘80s and ‘90s stretches across Michigan. Two health facilities, Beaumont and Spectrum, merged this year: the resulting 22-hospital system dethroned both Ford and General Motors as the state’s largest employer. Administrators have brought in consultants to cut $200 million per year. In some ways, the opposition facing healthcare unions is at its fiercest. But healthcare unions have risen to the occasion with equal intensity.
“Now is really a particular time, don’t you think?” muses Fairman. As nurses leave the profession in record numbers because of the conditions of the pandemic, she believes hospitals and the public are at last beginning to understand nurses’ value. They might just be able to change the course of healthcare if they are able to seize the moment as a collective. “Hospitals exist—and this should have been recognized so long ago—hospitals exist because people need nursing care. And nurses are really the linchpin of what happens in those institutions,” she says. “So, this is nurses’ time.”
Eva Rosenfeld is a writer and artist from Michigan.